When she was 33 weeks pregnant, Laura Avett told her obstetrician about a bizarre sensation she was having. “I know this sounds ridiculous,” she recalls saying, “but at times I feel like the baby is going to fall out of me.”
It wasn’t ridiculous at all. An assessment showed that Laura’s cervix was already dilating. She had signs of preeclampsia (a pregnancy-related condition characterized by high blood pressure) and was at risk for preterm labour (delivering the baby before 37 weeks). The doctor put Laura on strict bedrest to help prevent premature delivery: she had to remain lying down at all times, preferably on her left side, getting up only to use the washroom.
Dr. Jennifer Schnarr, an obstetrician/gynecologist in Kitchener, Ont., says is, “due to the fact that a preterm birth can have such devastating consequences, many healthcare providers will recommend bedrest in an attempt to reduce the risk as much as possible.” A 2008 survey published in the Journal of Obstetrics and Gynaecology Canada found that 65 percent of responding obstetricians and 70 percent of responding family physicians had
recommended bed rest for patients at risk of preterm birth. The World Health Organization’s 2012 report, Born Too Soon, says: “It is important to ensure that babies get at least 39 weeks of gestation when medically possible. A healthy baby is worth the wait.”
While the goal of any pregnancy is to reach full term, bed rest may not be the answer in every case. “The evidence supporting bed rest in the prevention of preterm birth is debatable,” says Dr. Schnarr. “Being confined to bed, especially during pregnancy, is not
without risk.” Physically, a pregnant woman’s inactivity may increase her chances of developing blood clots. Emotionally, it may cause feelings of frustration, isolation and anxiety.
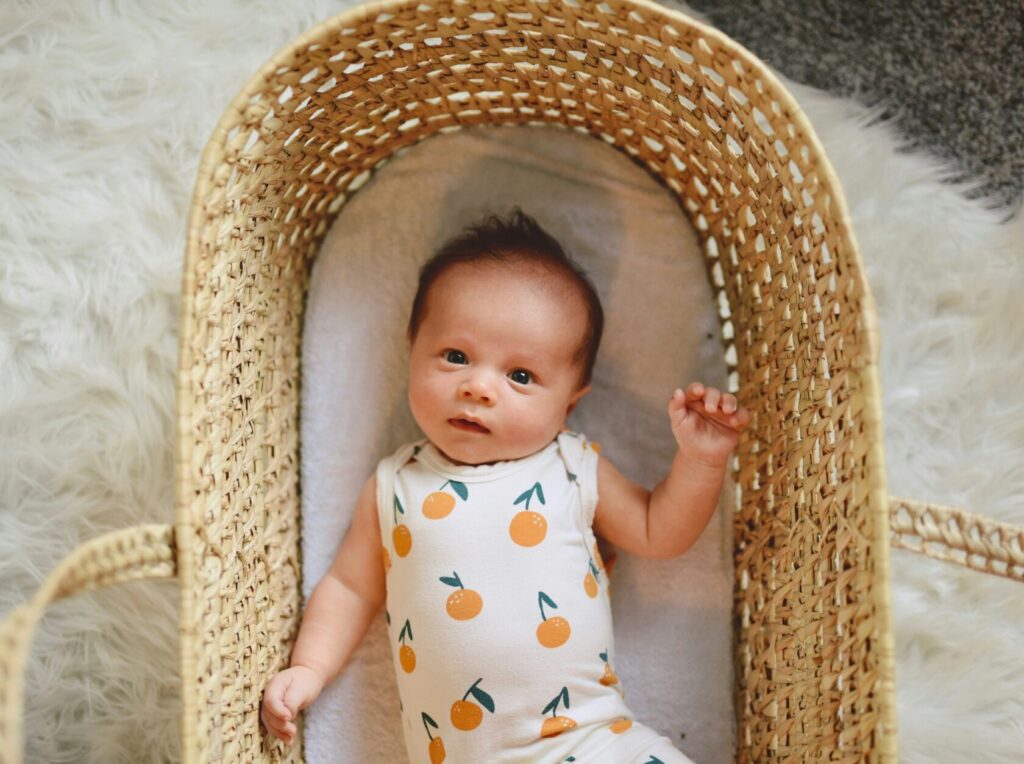
In Laura’s case, she followed her doctor’s instructions dutifully. She went on early maternity leave and relied on her husband and mother to look after her two-year-old daughter. Her blood pressure stabilized and her morning sickness subsided. Six weeks
later, at 39 weeks, Laura’s daughter Ella was born with no health concerns or complications. “My six weeks of bed rest now feel like a brief pause in my life,” says Laura. “It was a short period of time to sacrifice, given the impact it had on my child’s health.”
Coping with bed rest
- Obstetrician/gynecologist Dr. Jennifer Schnarr says: “Resting isn’t usually the difficult part of having a high-risk pregnancy. The difficult part is determining how to accomplish the activities of daily living such as cooking, cleaning and caring for older children.” She advises her patients to seek out support and accept help from relatives and friends.
- A smartphone or tablet can be a valuable lifeline. It’s a way to stay connected to friends and family, as well as gain access to online support groups.
- Counteract the worries and emotional strain by working on positive thinking. “It was hard because I was concerned about my baby being born too early,” says Laura Avett. “I woke up each morning wondering if today would be the day I would go into labour. Each night I remember having a little celebration in my head that I made it another day, which gave the baby more time to grow and develop.”
Originally published in ParentsCanada magazine, April 2013.