My birth plan seemed simple – to have
minimal medication and intervention during
labour. But come delivery day, it was anything
but simple. At 41 weeks I went into “stalled
labour.” After a Pitocin-powered induction, 18
hours of labour and two epidurals, I delivered
our baby via C-section. That was definitely not
in the birth plan.
A birth plan is a written document for the
medical team providing your care. “A birth
plan helps both sides know exactly what is
expected,” says Lisa Knapp, a labour and
delivery nurse at St. Alphonsus Medical Center
in Ontario, Ore. “It can provide a sense of
control to the couple over the birthing process,
and can ease the mother’s mind knowing that
if she becomes too overwhelmed during labour,
her wishes have already been communicated.”
Specifically, your birth plan should outline
the interventions you are comfortable or not
comfortable using. Epidurals, episiotomies,
induction and pain relief options should all be
considered and spelled out. Also important is
the aftercare of your baby – whether you want
skin-to-skin contact and how you want to feed
your baby.
Teresa Bandrowska, a certified nurse
midwife (CNM) with the Midwifery Group
of Ottawa, explains that the birth plan “can
clarify what is, or is not important to the
parents and offers the opportunity to discuss
their preferences and what can happen if
things deviate from the plan.” It is essential
to have several conversations about the birth
plan with your care provider, as “plans” may
require modifi cation.
Lisa says, “When the plan of labour is traded
for a long, painful, physically and mentally
exhausting labour that ends in a stressful
emergency Cesarean-section delivery, it can
naturally lead to a sense of disappointment.”
Lisa encourages parents to design a birth
plan that prepares for contingencies and
emergencies. “In a hospital setting there
are protocols that must be followed and
interventions are set in motion within seconds
if the baby is showing signs of distress.”
A lot of first-time moms put pressure on
themselves. Lisa says, “When things do not
go according to plan, there are some women
who feel they have failed. It is important to
encourage positivity but also to let the woman
voice herself and grieve her expectations. No
two deliveries are the same and it is hard to
plan for the unexpected.”
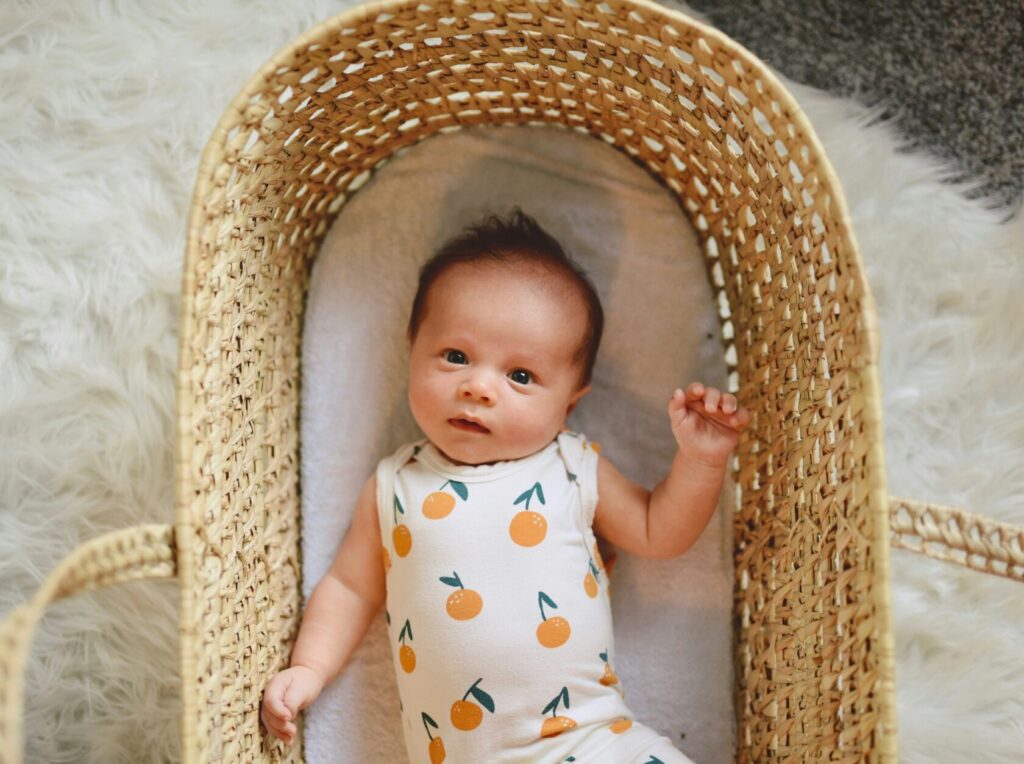
Both Lisa and Teresa emphasize the
importance of the end result – a happy, healthy
mom and baby – and sometimes that means
deviating from the plan.
Seek out support after a difficult delivery
- “Most communities have experienced therapists
and groups dedicated to reproductive counselling,
psychotherapy, hypnotherapy and other modalities for
healing trauma,” says Teresa Bandrowska, a CNM with the
Midwifery Group of Ottawa. “Most of these (resources)
have meetings and workshops that can greatly help a
woman come to a peaceful resolution.” - Lisa Knapp, a labour and delivery nurse, suggests
seeking out support “from family and friends who are
willing to listen. It can also help to find another mom who
may have had a similar experience. There may be “Mommy-and-Me” groups that can become invaluable to the new
mom. The woman’s doctor is another great resource who
can connect the woman and her family to a counselor.”
Originally published in ParentsCanada magazine, July 2013.